Paper presented to ‘TeleMed & eHealth 2008’, Royal Society of Medicine, London, UK, November 2008.
Robert J Marchbanks PhD 1 Edward F Good MD 2
1. Neurological Physics Gro up, Southampton University Hospitals NHS Trust, Southampton SO16 6YD, UK.
2. Neurological PI, NASA Experiment E148, Johnson Space Center, Houston, USA.
Author for Correspondence
Robert Marchbanks Neurological Physics Group,
Southampton General Hospital,
Southampton University Hospitals NHS Trust,
Southampton, SO16 6YD, UK.
Email robert.marchbanks@suht.swest.nhs.uk
Declaration
Dr Robert Marchbanks is the Managing Director of the medical research -based company, Marchbanks Measurement Systems Ltd.
Summary
The main aim of this paper is to highlight the synergy between the remote care requirements for NASA and community/rural based medicine. It demonstrates the appropriateness of applying similar health -care models for space -based medicine as for ‘2020 vision’ community -based medicine and the common use of screening devices with telemedicine capabilities. There is a requirement to diagnose and manage complex cases remotely and the need to empower on -site medically trained personnel to undertake the physiological measurements and decision – making. The common aim is to reduce the need for hospitalisation — in both cases the issues are logistics, convenience and cost. For NASA hospitalisations become major issues if the crew member needs to be returned to earth from Space Station or the proposed lunar base. For space exploration at greater distances, the telemedicine systems used will require added sophistication to support autonomous cre w medical screening, diagnosis and interventions (Williams etal 2000).
Non -invasive Cerebral and Cochlear Pressure Assessment
By means of an example, we will first consider our own medical device for non -invasive cerebral and cochlear pressure assessment. This device , the tympanic membrane displacement (TMD) technique, provides a good indication of cerebral pressure variations from the cardiac and respiratory cycles and also a qualitative assessment of baseline intracranial pressure (ICP) (Lin et al, 2005; Marchbanks, 2003; Lehrer etal, 2007). TMD is a quick, safe and painless test that uses a transducer positioned in the patient’s ear canal to measure movement of the tympanic membrane. It has been shown that ICP is in communication with the inner ear via the cochlear aqueduct and that inner ear pressure waveforms replicate the ‘signature’ of the ICP waveform. Inner ear pressure is transmitted via the bony ossicles into movement of the tympanic membrane and therefore the tympanic membrane movement reflects ICP changes. Ours is the only non -invasive measure of ICP in routine clinical use for assessment of cerebral and cochlear pressure, and recently it has been included by the UK Department of Health in their commissioning healthcare pathways. Clinical applications include patients with neurological disorders and those with neurosurgical treatments, such as intraventricular shunts. We also provide a specialist clinical service for patients with balance, tinnitus and hearing problems where ther e is doubt concerning the clinical diagnosis. We are active in a number of research areas and these include collaborative research with the Kenya Medical Research Institute into cerebral malaria, and collaborative research with NASA as will be described further.
NASA Space Exploration
Our TMD Technique has been adopted by NASA to investigate changes in intracranial pressure pre -flight, in space and in the post -flight period. The purpose of the NASA experiment E148, is to correlate symptoms of space adaptation syndrome (SAS) with intracranial pressure (ICP), as the ICP is known to increase with reduced gravity that results in a head -ward movement of body fluid. If a correlation between SAS and ICP is found, then it will be possible to suggest countermeasures to ameliorate SAS. Our non -invasive ICP assessment is designed for use on the NASA Space Shuttle, however, with the imminent retirement of this space vehicle, it is now listed as device for an International Space Station experiment. The adoption of name that may be familiarised by NASA crewmembers is commonplace and our ICP measurement platform is referred to as ‘Old Peculiar’.
In addition to non -invasive assessment of static and dynamic ICP, Old Peculiar includes middle ear assessment by tympanometry and ‘reflexometry’ and is integrated with flight -approved equipment for measurements of ECG and continuous blood pressure.
The proposed long -term objective of ‘Old Peculiar’ is regular assessments of neurological and audiological function so as to monitor any effects of gravity transitions and long -term exposure to zero or lunar gravity, cosmic radiation, breathing regimes and other environmental factors. Hearing disorders or damage is likely to result in auditory communication deficits and ICP abnormalities are frequent associated with disorders such as ‘brain -fog’ and cognitive deficits. The combination of these disorders greatly increases the risk of misinterpreting commands, and consequently may precipitate incidents and major accidents. Future NASA space exploration will involve crews being in space for much longer periods of time and in location such as a permanent Lunar base and Mars that are at significantly greater distances from Earth.
It is envisaged, therefore, that the long -term objectives of ‘Old Peculiar’ is to provide a neuro-otologic screening and a diagnostic capability in the case of disease or trauma, and to provide an alternative neurological assessment in the absence of brain scanning or continuous ICP measurement techniques. It is proposed that the long -term benefits of using ‘Old Peculiar’ would be: – more accurate diagnosis of disease or accumulating physiological deficits; early and more specific implementation of countermeasures (treatments); reduced risk of major incidents or disasters; improved in-situtriage and clinical assessments, therefore avoiding unnecessary returns to Earth. NASA Timeline for Human Space Exploration is is 2014 for commissioning of the new NASA launch system called Constellation; the ‘2020 vision’ is to establish a permanent Lunar base; between 2030 and 2040 it is anticipated that a human landing on Mars will occur. The most immediate objective is the return to the Moon and this poses the possibility for complex neurological and neuro-otologic remote care.
Future Earth -Based Healthcare
Wherever possible patient care needs to be undertaken at primary healthcare level and within the community. There is a requirement for new medical screening devices that have a telemedicine capability. These devices should facilitate reliable and cost -effective triage at primary healthcare level, and have a positive impact on the huge social -economic costs of the long -term care of patients with familiar chronic medical conditions. We have built telemedicine equipment based on the TMD technique for NASA that screens for complex neurological and oto -neurological conditions. These conditions are suffered by some of the major patients groups – US and European estimates are that 2 to 3% of the popula tion are suffering the long -term/life -time effects of brain injuries such as traumatic brain injury (TBI); 30% of patients visiting a primary -care doctor complain of dizziness or vertigo. The TMD is currently included in the UK Department of Health, 18 we ek Commission Pathway – Dizziness 2008. It is applied under ‘subspecialist’ assessment according to the ‘Red Flag’, diagnostic doubt, and is used for diagnosing intracranial hypertension as the basis for certain audiovestibular disorders. The long -term objective is to establish by means of clinical trials TMD assessments at primary health care level for screening and the management of patients with long -term/life -long chronic conditions, namely dizziness, chronic headache, traumatic brain injuries and (TBI), other brain malformation or injuries. As with our NASA device, this will combine multi -physiological measurement inputs with a telemedicine capability. It is proposed that such screening assessments with TMD will help to: – Improve clinical triag e at primary care level by identifying neurological disorders that currently slip through the ‘triage net’. Avoid referrals to inappropriate specialties. Avoid premature diagnosis that can greatly delay referrals to specialties or even ‘fix’ patient man agement at primary health care level. Avoid the risk of ineffective and possibly costly treatments. Avoid the onset of secondary psychological disorders know to occur with delayed diagnosis and ineffective treatments. Research demonstrates that 66% of dizzy patients in tertiary clinics had suffered psychiatric symptoms in a 3-4 year review period (Eagger et al, 1992).
Healthcare Models
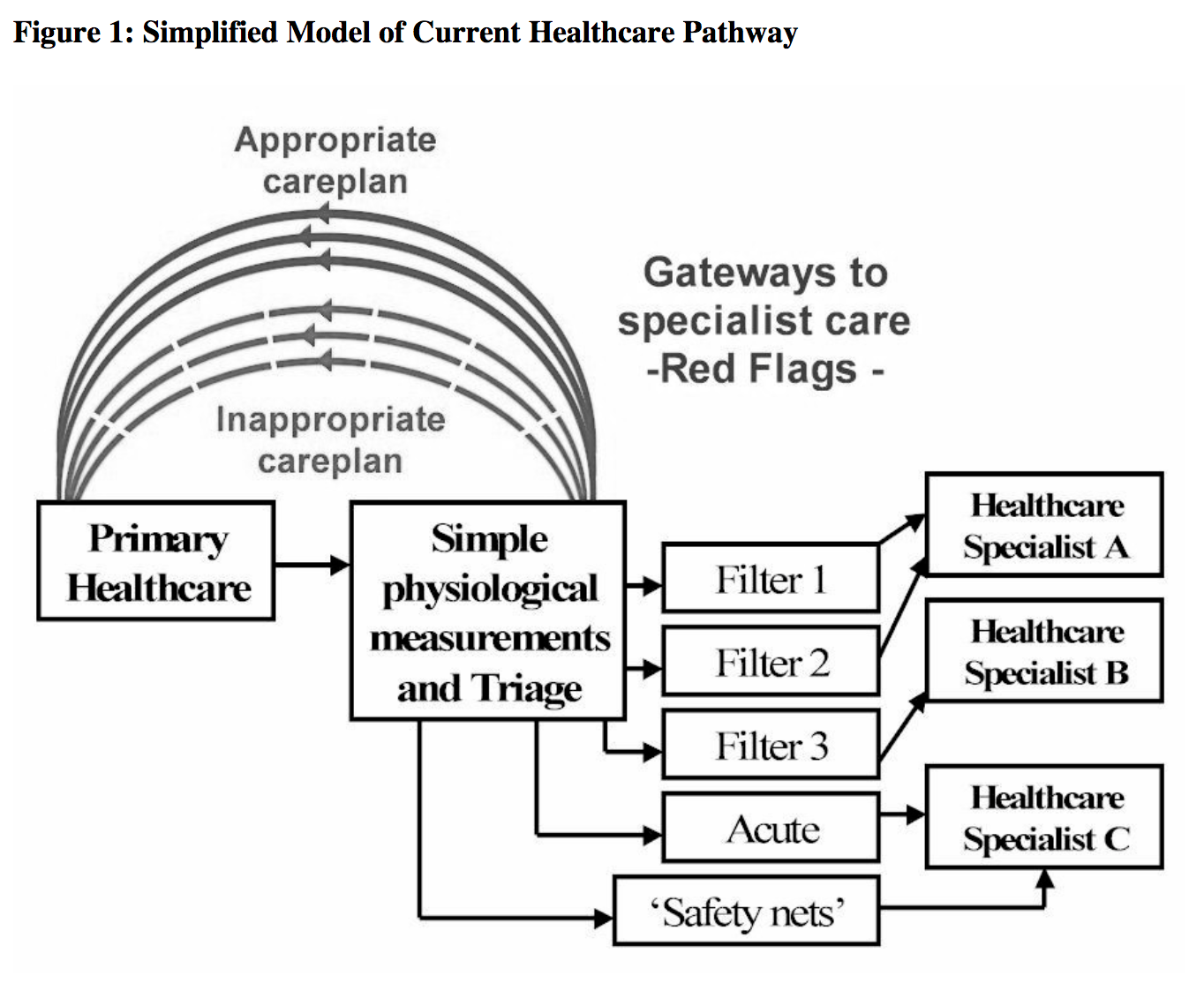
The current healthcare trend is from acute to chronic care, and consequently the present healthcare model is considered to be unsustainable under the 2020 vision. Healthcare trends in general reflect a need and an increasing expectation that diagnostic assessments that are currently undertaken at the tertiary/specialist level, should be undertaken at an earlier stage in the patient care pathways, and wherever possible, during primary assessment. This will help to refine and improve care pathways, is logistically better for the patient and their carers, will assist with earlier diagnosis and treatment, and is anticipated to reduce individual patient management costs at a time when overall healthcare costs are escalating. It is valuable to visualise the current healthcare model, together with the likely ‘2020 vision’ Earth and Space – based models. Figure 1 represent s a simplified representation of the current healthcare pathways. In practise, the care pathways have three principle levels; however, only two are included here to emphasis the primary healthcare aspect. Included is the concept of ‘gateways’ to more specialist levels according to compliance with ‘red flag’ filters, acute conditions and ‘safety nets’ for ‘diagnostic doubt’. Present healthcare models are largely stochastic, that is, the ‘gateways’ have in the main been determine according to a ‘consensus of expert opinion’ and in accordance with an ‘evidence -base’ that is a statistical representation of patient condition. A proportion of the patient s will not pass through the gateways to more specialist care levels and an appropriate careplan will be provid e at primary health care level. However, an inevitable consequence of this methodology is that a significant proportion of patients will fail the gateways and incorrect diagnosis or inappropriate management/treatment will occur at primary level. This is schematically represented in figure 1.
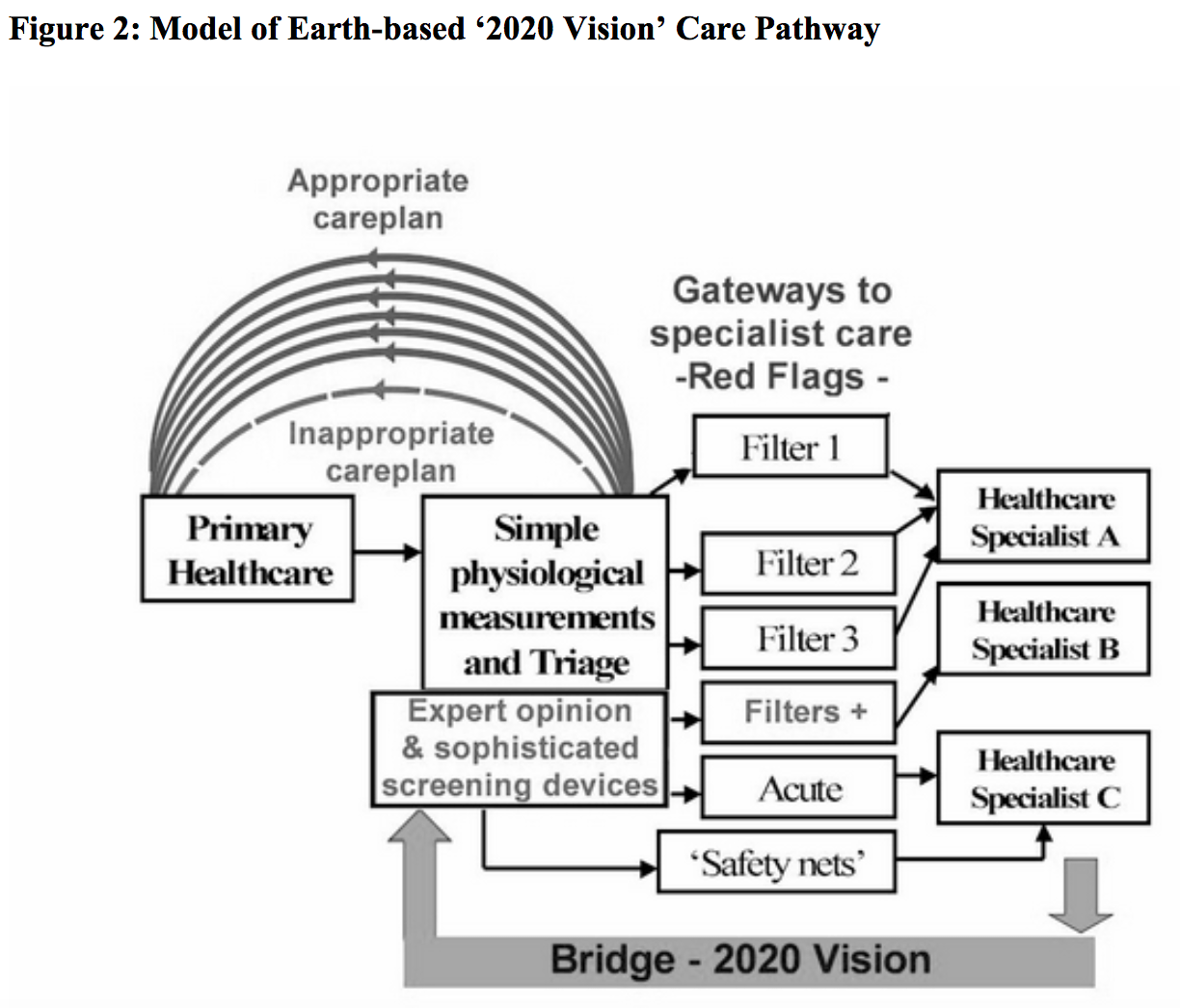
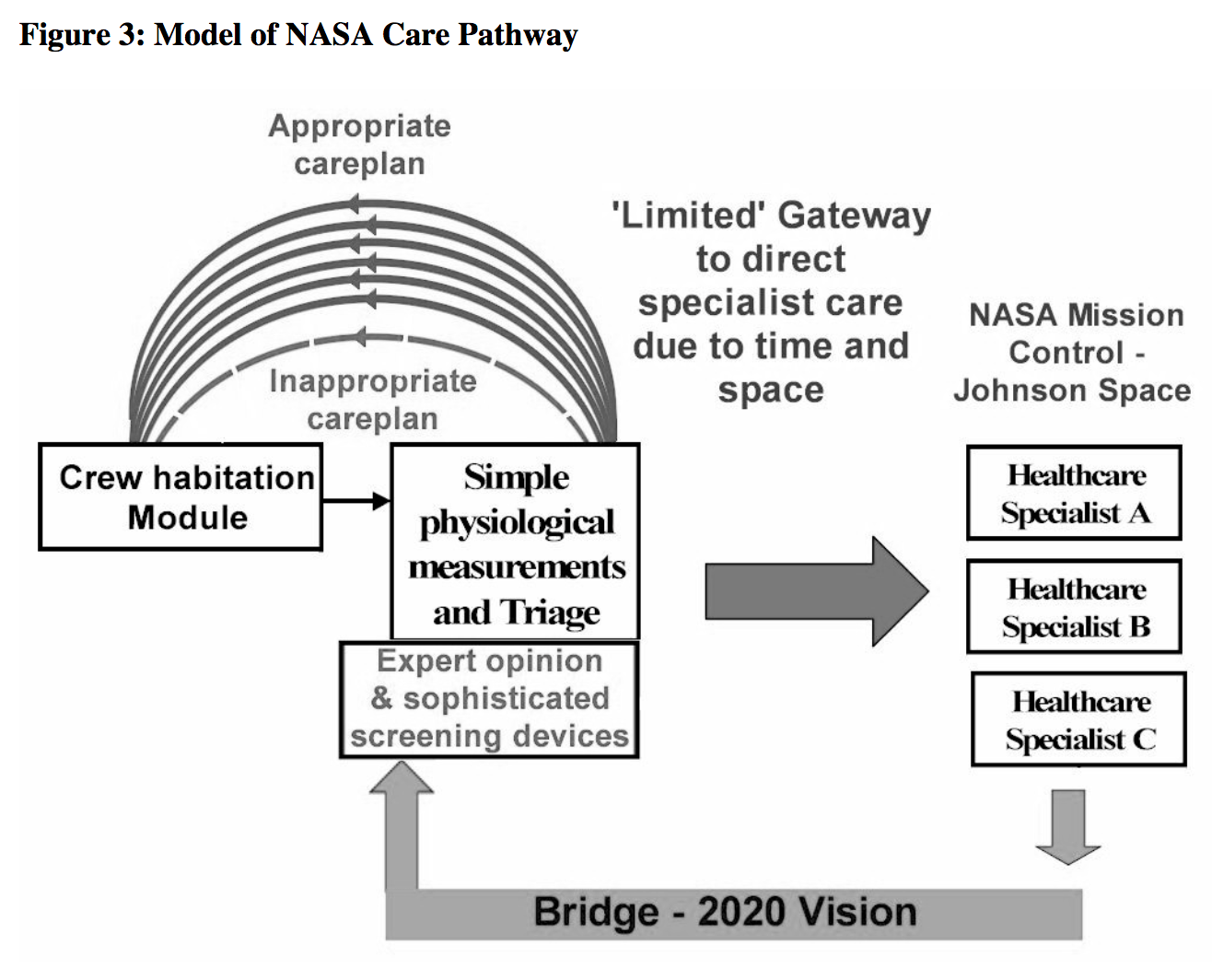
In contrast a ‘2020 vision’ model is better ‘tuned’ on an individual patient’s needs by introducing a ‘bridge’ for individual ‘expert opinion’ and sophisticated screening devices prior to the gateways, figure 2. The ‘expert opinion’ aspect will exist as a consequence of an evolutionary process that is driven by innovation and not simply a medical consultant specialist with a video link. Likewise, sophisticated screening devices will embrace techniques currently existing at specialist care levels with the addition of major innovations currently in the pipeline or yet to be discovered . These are likely to have telemedicine capabilities. The benefits of adding expert opinion and sophisticated screening devices are to: – Increase the number of ‘red flags’ and ‘gateways’ to specialist healthcare. Avoid referrals to inappropriate specialities. Increases the number of patient cases that can be managed at primary healthcare level. Reduces the number of inappropriately managed patients at primary healthcare level, i.e. inappropriate ‘Gateway’ failures. Our model of the NASA care pathway for is given in figure 3. Whether Earth or Space -based, a ‘2020 vision’ recognises the require ment for specialist expertise and sophisticated screening technology to be integrated at primary care level or at remote space locations. Important synergies exist between the Earth -based healthcare in 2020 and healthcare that is suitable for long -term space exploration missions . The ‘Gateways’ to the specialist healthcare levels represent the transposition of an individual space -traveller to Earth versus ‘transposition’ of significantly number of patients to specialist care respectively. Both have major cost and logistical implications. Although beyond the scope of this paper, it is important to recognise that NASA healthcare systems are build on a foundation that is a quality system. It is to be expected that ‘2020 vision’ healthcare delivery will also be underpinned by a quality system.
Principal factors common to Earth -based and Space -based referrals to specialist care centres are appropriateness and logistics, distance and time, locomotion issues and risks, inconvenience, and costs. The requirements common to both are: – A degree of autonomy Teleconferencing link with medical specialists Effective diagnostics leading to appropriate patient/crew member treatment and management ‘Well -tuned’ triaged integrated with ‘easily -applied’ physiological measurements Sophisticated screening equipment Minimal operator training periods Professional but non -technical/specialist operators High level of reliability, i.e. fault tolerance Ease of operation – minimal training time Robustness
Overcoming Barriers to Implementation
Evolutionary design changes or merely adapting existing medical equipment for use as primary care screening devices may only have limited success. In the main, only innovative designs will meet the full list of require ments noted above. This entails manufacturers implementing new design processes, whereby the requirements are the starting point and from this, an equipment specification is defined. Screening equipment for community management of complex chronic conditions needs to be simple in application but is likely to be complex in design, using multi -physiological sensors inputs in combination with complex software algorithms. This will present implementation barriers since manufacturers will need significant resources both financially and in terms of highly skilled design engineers and scientists. High design costs stem from the need to ensure robust and highly reliably equipment, integral fault tolerance of incorrect/deviant operation, and the need for a level of autonomy. Furthermore, equipment with radically new designs will necessitate full design documentation with testing to meet regulatory requirements, and are likely to require validation through clinical trials Although development costs are likely to be high, the market price of screening devices to primary care will be relatively low. The manufacturer will, therefore, consider the ‘bringing to market’ of sophisticated screening devices as a high -risk venture.
Who will Pay?
Funding and proactive involvement by stakeholders will be required to ensure screening medical devices are developed that meet ‘2020 vision healthcare’ . To ensure success, there will be a need for collaborative partnerships between industry, universities and international government agencies including health services, departments of defence and homeland security, and space agencies such as NASA. There is a need for exemplary pilot studies for medical screening devices that have a telemedicine capability. In addition to the NASA project, I would like to acknowledge the importance of our partnering of research in Kenya (KEMRI -Wellcome Research Programme http://www.kemri -wellcome.org/ ) where our technique is being piloted for the diagnosis and acute care management of comatose children with cerebral malaria.
Further information;
– http://www.medphys.soton.ac.uk/randd/Clinical/neuro/non-in.htm
– https://www.marchbanks.co.uk
References and Bibliography:
Eagger S, Luxon LM, Davies RA et al. (1992). Psychiatric morbidity in patients with peripheral vestibular disorder: a clinical and neuro-otological study. J Neurol Neurosurg Psychiatr. 55:383 -387.
Lehrer JF, Ogunlusi A, Knutsen J (2007). Applications of the Marchbanks Transcranial -Cerebral Sonography Technique in Neurootology: Preliminary Report. International Tinnitus Journal 13 (1): 41-44.
Lin JP, Rosenthal E, Marchbanks R. (2005). Non -invasive assessment of intracranial arterial and respiratory pressure waves via the trans aural route in man. Proc. Physiological Society Kings College London J Physiol 19:565.
Marchbanks RJ (2003). Measurement of inner ear fluid pressure and clinical applications. Chapter 17, pp 289 – 307. In ‘Textbook of Audiological Medicine: Clin ical aspects of hearing and balance’. Ed L.Luxon. Martin Dunitz Ltd. 2003, ISBN 1-90186 -534 -7.
Williams DR, Bashshur RL, Pool SL, Doran CR, Merrell RC, Logan JS (2000). A strategic vision for telemedicine and medical informatics in space flight. Telem edicine J and e-Health 2000; 6 : 441 -448

